
A blog from Dr Cheryl Crocker, AHSN Network Patient Safety Director, describing how Patient Safety Collaboratives (hosted by the AHSN Network) are supporting people to manage their long-term pain and reduce the harmful effects of opioid medication.
Opioids are highly effective medications and, when used judiciously for a time-limited period, can greatly benefit many people living with pain.
When it comes to long-term pain (also called “chronic” pain) that is not associated with cancer, the National Institute for Health and Care Excellence (NICE) guidance states that opioids should not be offered as an option to patients because the harms outweigh the benefits.
The Faculty of Pain Medicine (FPM) advises that using opioids for longer than three months can do more harm than good. Because the risk increases further with higher doses, the FPM advises that increasing the dose to greater than 120mg per day (of oral morphine equivalent) is unlikely to benefit patients further.
Despite this, a review carried out by Public Health England in 2019 showed that during 2017 and 2018, half a million adults in England had been prescribed opioid pain medicines for three years or more. More recently, in January 2021, over one million people in England were prescribed opioids for more than three months (NHSBSA).
The good news is that healthcare professionals and communities have risen to the challenge. At the end of 2021/22, a “real world” intelligence gathering exercise was undertaken by AHSN-hosted Patient Safety Collaboratives, supporting the NHS Patient Safety Strategy. This exercise identified 112 separate instances of services working to reduce opioid prescribing.
Drawing together the learning allowed the development of a whole system approach to reduce harm from opioids and help people to live well with chronic non-cancer pain. Local stakeholders came together to share an understanding of the challenges, identify the greatest opportunities for change, and work together as a network to implement sustainable long-term solutions.
In 2022, using the whole systems approach, the Patient Safety Collaboratives (PSCs) began to work with integrated care systems (ICSs) to understand how chronic pain and opioid prescribing affect local people by mapping the current system. In particular, attention was brought to the importance of doing this with stakeholders who don’t have an NHS badge, community groups and patients. This also helped to develop understanding of other ways to support people to live well with pain.
The ambition of this programme is that by the end of March 2023, PSCs, working with a minimum of 15 ICSs, will implement a whole systems approach to high-risk opioid prescribing framework, with the following collective outcomes:
- 30,000 fewer people prescribed oral or transdermal opioids (of any dose) for more than three months.
- Of the 30,000 above 4,500 of these people will have been prescribed a high dose (>120mg day OME) at baseline.
The whole systems approach was launched in January 2022. Between January and October 2022, an average of 21,520 fewer people per month were prescribed oral or transdermal opioids (of any dose) for more than three months, compared with the baseline period of January 2021-December 2021.
This translates to:
- As many as 347 fewer people who might die over the next 2 years.
- 2,152 fewer cases of short term harm per year.
Patients report better quality of life, less pain and less disability as a result of improved care.
PSCs are supporting 24 ICSs through the whole systems approach framework. A further eight ICSs are being supported by PSCs through sharing the learning.
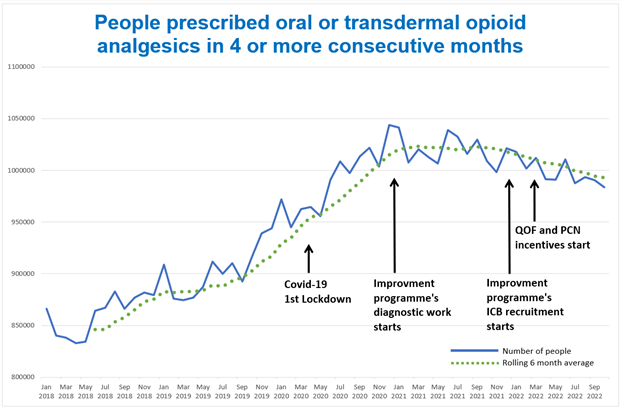
Data source: NHSBSA PAIN03 metric at a monthly level for National organisational structures, NHSBSA Copyright 2023.
The AHSN Network’s national polypharmacy programme is a further example of a programme which brings health systems together, in this instance, to identify patients at greatest risk from harm from problematic polypharmacy. The programme supports clinicians to carry out better medication reviews with greater patient involvement and is particularly focused on patients aged over 75 who are taking 10 or more medicines regularly.
Both programmes are underpinned by a number of key elements
- Using prescribing data to prioritise patients deemed to be at greatest risk of harm.
- Empowering patients as partners in structured medication reviews, where shared decision-making is at the core of the consultation between the clinician and the patient.
- Supporting health systems to work together on tackling these complex issues.
When asked to share his perspective on the subject, Tony Jamieson, NHS England Patient Safety Specialist & Clinical Improvement Lead for the Medicines Safety Improvement Programme said:
“Together, we are saving lives, preventing harm and helping people who live with chronic pain to reclaim the lives that have been stolen from them by opioid analgesics. The lives that have been saved in this programme have been the result of wrapping local, regional and national support around patients, their communities, clinicians and system leaders.
“It is a ‘whole-system’ approach, starting with national collaborations to align policy drivers and deliver national learning opportunities. These enable integrated care partnerships to lead change locally being supported by the AHSN Patient Safety Collaboratives, experts in safety science and systems thinking.”
We are delighted to work with NHS England Patient Safety Team and system partners to improve the lives of people with chronic, non-cancer pain and are now seeing the benefits. There are many examples of excellent practice across the country including co-design and co-production with patients resulting in improved pathways of care.

There is a wealth of HealthTech innovators poised to help solve some of the NHS’ greatest challenges, yet getting a product or new technology adopted at scale in the NHS is far from straightforward. In a recent ABHI member’s survey*, procurement was cited as one of the biggest barriers that innovators face, particularly those from [...]

Tellmi is a social enterprise innovation which aims to address the growing demand for mental health services and tackle health inequalities for young people. It is a digital peer support app available launched in 2017 by psychologist Suzi Godson PhD and engineer Kerstyn Comley PhD. Kersytn explains how Tellmi works. Tell us about the innovation. [...]

The NHS is facing record demand for services. According to The Health Foundation, the NHS waiting list for elective treatment in England has almost tripled in size over the last decade to 7.7 million. And latest figures show there were a record 2.35 million attendances at A&E across England in March this year. We know [...]







