It was World Patient Safety Day on Saturday 17 September, and this year the World Health Organisation (WHO) is focusing on medication safety.
This is a welcome theme for the AHSN Network and the Patient Safety Collaboratives (PSCs) we host as improving medication safety is a key objective in our Patient Safety Plan, which we updated earlier this year and sets out our commitment to contributing to the NHS Patient Safety Strategy.
One of our new national AHSN Network adoption and spread programmes outlined in our Patient Safety Plan is tackling problematic pharmacy.
It has been estimated that there are around 237 million medication errors in England every year. Thankfully, many do not lead to patient harm but up to 66 million of these are clinically significant. Avoidable adverse drug reactions cost the NHS approximately £98.5 million per year, consuming 181,626 bed-days, causing 712 deaths, and contributing to a further 1,708 deaths according to 2018’s EEPRU report.
The WHO’s third global health challenge, Medication Without Harm, has set out to reduce severe avoidable medication-related harm by 50%. The WHO highlights that as medicines are the most common therapeutic intervention, ensuring safe medication use and having the processes in place to improve medication safety should be considered of central importance to countries working towards achieving universal health care.
Medication safety in polypharmacy has been identified by the WHO as one of three key areas where early action and effective management could reduce harm, which is what our new national programme aims to address.
Polypharmacy: Getting the Balance Right
Polypharmacy simply means many medicines and refers to the issues that arise when people take medicines for multiple long-term conditions. As indicated in the NICE: Medicines Optimisation Quality Standard, this becomes a bigger problem with an ageing population as 25% of people over 60 have two or more long-term conditions and 30-50% of medicines prescribed for long-term conditions are not taken as intended.
Studies have shown that over 50% of older people are prescribed a medicine where the harm outweighs the benefits, leading to morbidity, hospitalisation and mortality. In addition, the most deprived areas tend to have the most issues around polypharmacy, making this a health inequality issue.
The national AHSN Polypharmacy Programme: Getting the Balance Right <link to PAGE NUMBER 33> is a three-year programme, launched in 2022, which is creating clinical, multi-stakeholder communities across England, focussing on the issue of problematic polypharmacy within their local geographies.
The programme is based on three core principles: population health management, education and training, and public behaviour change. Work includes supporting local health systems in identifying patients at risk of potential harm from polypharmacy, supporting better conversations about medicines, and providing education and training on polypharmacy for GPs and pharmacists.
This work builds on the AHSNs’ strong history in polypharmacy in the creation of England’s first polypharmacy national data set, the NHS BSA polypharmacy prescribing comparators.
Improving non-cancer related chronic pain management
Our Patient Safety Plan also includes the five national patient safety improvement programmes, commissioned by NHS England. One of these is the Medicines Safety Improvement Programme, which is working towards the goal to reduce opioid prescribing for non-cancer chronic pain by 50% by 2024.
Most of the 0.5 million people in England who are prescribed opioid medications for longer than three months have non-cancer related chronic pain. Whilst opioids can be of great benefit to those living with pain, the risks can outweigh the benefits, particularly in longer-term use. Around 6,000 people a year are hospitalised with adverse events whilst taking opioids for extended periods (NHSBA).
Hear about Paul Hemsil’s experience of living with chronic pain in the video below:
Alternative ways of managing this type of pain need to be shared, and to facilitate this, Patient Safety Collaboratives (PSCs) conducted a research project across England. Following a scoping exercise, 15 PSCs worked within their local systems to identify real-world projects to improve chronic pain management. Stakeholders from a range of areas including medicines optimisation, pharmacy, acute and primary care teams, drug and alcohol teams, the third sector and academics were engaged to help build a whole-system picture.
Leaders in Integrated Care Systems (ICS) can access this analysis to learn from other areas and find resources that will help as they design and deliver improvement programmes for people living with chronic pain. The report is titled: Improving chronic pain management by reducing harm from opioids and is available on the AHSN website <link to RESOURCE NUMBER R63> and also on the patient safety FutureNHS site which you can request access to by emailing NHSps-manager@future.nhs.uk.
Improving patient safety across the board
AHSNs hold deep relationships within local health systems, bringing a wealth of understanding of the issues on the ground in every area. Hosted by local AHSNs, Patient Safety Collaboratives are in an optimal position to translate evidence into real-world practice and use quality improvement approaches to facilitate sustained and embedded change.
The current programmes which Patient Safety Collaboratives are delivering in their respective AHSNs for 2022/23 are shown in the ‘driver diagram’ below:
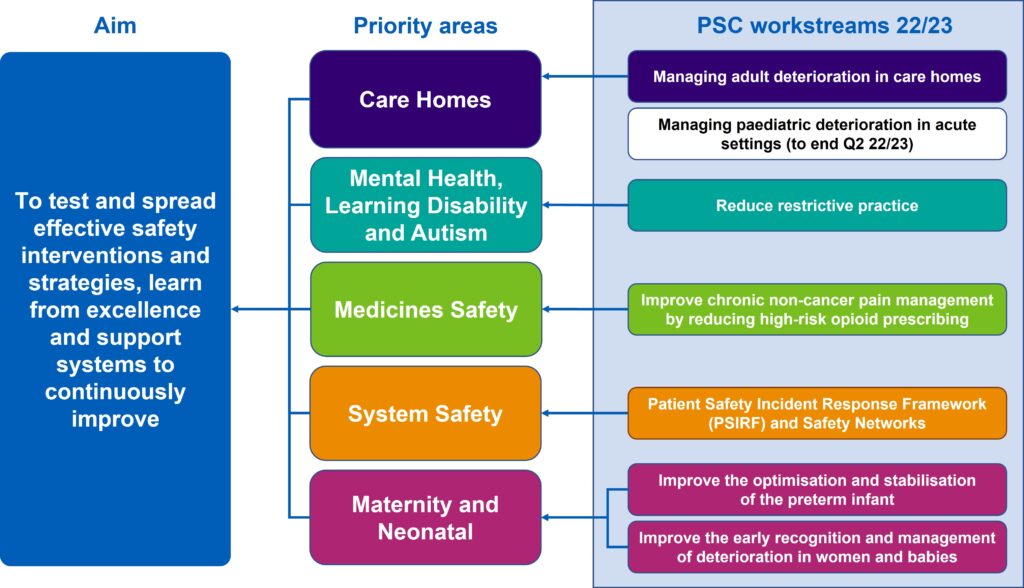
The AHSN Network is making significant progress in delivering the objectives set out in the NHS Patient Safety Strategy. A midpoint update to the AHSN Network patient safety plan has been released. This update shows the impact being made across its priority areas: care homes, mental health, system safety, maternity and neonatal, and medicines safety.
- Download the full update: Patient safety in partnership: Our plan for a safer future 2019-2025 – Progress report
- You can find your local AHSN to discuss support for patient safety where you work.
- Meet our polypharmacy programme team and contact Amy Semple, Programme Manager for the AHSN Polypharmacy Programme for more information.

There is a wealth of HealthTech innovators poised to help solve some of the NHS’ greatest challenges, yet getting a product or new technology adopted at scale in the NHS is far from straightforward. In a recent ABHI member’s survey*, procurement was cited as one of the biggest barriers that innovators face, particularly those from [...]

Tellmi is a social enterprise innovation which aims to address the growing demand for mental health services and tackle health inequalities for young people. It is a digital peer support app available launched in 2017 by psychologist Suzi Godson PhD and engineer Kerstyn Comley PhD. Kersytn explains how Tellmi works. Tell us about the innovation. [...]

The NHS is facing record demand for services. According to The Health Foundation, the NHS waiting list for elective treatment in England has almost tripled in size over the last decade to 7.7 million. And latest figures show there were a record 2.35 million attendances at A&E across England in March this year. We know [...]







