The Patient Safety Collaboratives (PSCs) have been working to deliver a programme aimed at reducing restrictive practice in mental health in-patient settings.
Work is underway with 14% of all NHS mental health, learning disability and autism wards across England, which equates to 172 wards. Reductions in restrictive practice use in now being seen in a number of wards. PSCs are also working with the five largest independent providers of care for NHS patients with mental health needs, learning disabilities and autism.
In 2015, the Mental Health Act Code of Practice called on mental health services to reduce restrictive interventions. These practices are used with mental health, learning disability and autism inpatient services to prevent individuals in these services from harming themselves or others. These practices should be a last resort because whilst they are used to prevent harm, research shows that they cause harm to patients experiencing them and to staff involved.
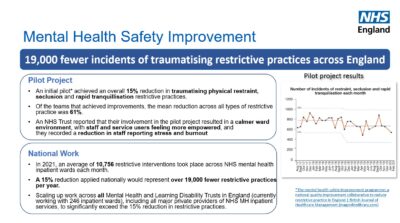
Restrictive practices include physical restraint, seclusion, and rapid tranquilisation. Reports have found that there is a significant variation in the way restrictive practice are being used when responding to challenging situations.
The Department of Health and Social Care’s Mental Health Units (Use of Force) Act 2018 statutory guidance of 2021 reports that there is still work to do. The Act aims to provide an opportunity to embed a consistent approach across services nationally. It encourages a trauma-informed way of working where the use of force is an uncommon experience for patients and staff.
The Mental Health Safety Improvement Programme (MHSIP) delivers the core changes described within this Act. The MHSIP supports staff and patients to work together to improve services and reduce the need to use restrictive interventions in their wards.
Led by NHS England and delivered by regional, AHSN-hosted, PSCs, the programme will continue to scale up and spread the reducing restrictive practice package. The package was developed for the MHSIP by the National Collaborating Centre for Mental Health (NCCMH) in a national reducing restrictive practice pilot group. MHSIP supports the NHS England Patient Safety Strategy.
The programme aims to improve safety by reducing harm caused to people using mental health, learning disabilities and autism in-patient services by 2023. The PSCs will focus on creating safer in-patient mental health and learning disability and autism services by using a systematic quality improvement approach to reduce restrictive practices delivered through our mental health safety improvement networks.
Initial indications show that a 15% reduction in restrictive practices across England would represent over 19,000 fewer incidences of restrictive practice per year.
*The mental health safety improvement programme: a national quality improvement collaborative to reduce restrictive practice in England
British Journal of Healthcare Management (magonlinelibrary.com)
Dr Cheryl Crocker, AHSN Network Patient Safety Director said:
“We are very excited to see how wards are improving their practices and reducing restraint. This has benefits for service users and staff. We will be sharing examples of the great work wards have done in the months to come. Our mental health safety networks are an excellent forum to share learning and support each other.”
Dr Helen Smith, Consultant psychiatrist and Clinical Advisor to the mental health safety improvement programme, commented:
“Nobody wants to receive care or work on a ward with high levels of restrictive practice, they are stressful and unpleasant places for everyone to be. This programme gives staff and patients the tools and the power to do something different and improve the safety of care for everyone. We are starting to see some significant sustained reduction in restrictive practice. Watch out for the inspiring stories that staff and patients are sharing as this programme progresses.”
- Find out more about the mental health safety programme.
- Read about PSCs and the AHSN Network’s patient safety plan.

There is a wealth of HealthTech innovators poised to help solve some of the NHS’ greatest challenges, yet getting a product or new technology adopted at scale in the NHS is far from straightforward. In a recent ABHI member’s survey*, procurement was cited as one of the biggest barriers that innovators face, particularly those from [...]

Tellmi is a social enterprise innovation which aims to address the growing demand for mental health services and tackle health inequalities for young people. It is a digital peer support app available launched in 2017 by psychologist Suzi Godson PhD and engineer Kerstyn Comley PhD. Kersytn explains how Tellmi works. Tell us about the innovation. [...]

The NHS is facing record demand for services. According to The Health Foundation, the NHS waiting list for elective treatment in England has almost tripled in size over the last decade to 7.7 million. And latest figures show there were a record 2.35 million attendances at A&E across England in March this year. We know [...]