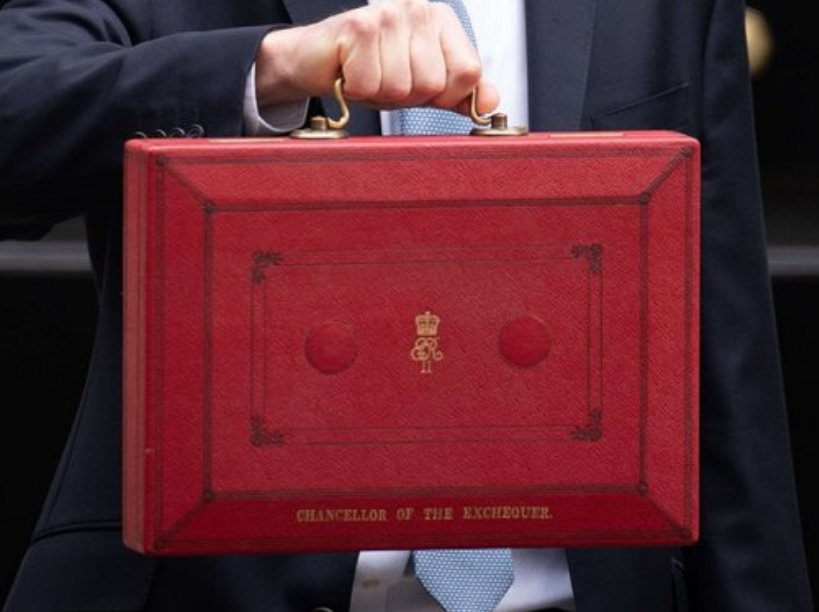
As part of the recent spring budget, Jeremy Hunt, the Chancellor of the Exchequer, announced a £3.4bn package for the NHS, specifically to increase productivity.
This included £430m to support digital transformation to increase access and improve services for patients, £1bn to transform the use of data and reduce time spent on administrative tasks, and £2bn to update IT systems, scaling up the use of artificial intelligence (AI) and digital.
During his statement to the House of Common, the chancellor said: “When we published the NHS Long Term Workforce Plan, I asked the NHS to put together a plan to transform its efficiency and productivity. I wanted better care for patients, more job satisfaction for staff and better value for taxpayers.
“Making changes on the scale we need is not cheap. The investment needed to modernise NHS IT systems, so they are as good as the best in the world costs £3.4bn. But it helps unlock £35bn of savings, ten times that amount.”
The Health Innovation Network is commissioned by NHS England to help the NHS to discover, develop and deploy new ideas, innovations, improvements, and best practice to benefit more patients faster. Many of the innovative solutions we work with don’t just deliver patient benefit, but help to increase productivity, reduce administrative burden for clinicians and ensure better use of resources.
If spread and scaled appropriately, these innovative solutions have the potential to help the NHS to deliver the ambitious 2% increase in productivity that the government funding is reliant on.
The challenge set out by the chancellor is to use digital health technologies, including AI to increase productivity. Health innovation networks have a database of thousands of innovations that are in different stages of development. Taking a handful of examples we look at how new technology solutions can help the NHS with its productivity plan.
C2-Ai – Automated Patient Tracking System
C2-Ai is helping hospitals improve patient safety, reduce mortality and complication risk, and clinical outcomes variation, by providing globally unique AI-backed insights. It also provides the opportunity to improve productivity by reducing and streamlining patient wait lists.
With support from Health Innovation North West Coast, Cheshire & Merseyside ICS was the first to implement C2-Ai’s Patient Tracking List (PTL) triage system across the system. This resulted in saving in saving 125 excess bed-days per 1,000 patients on the PTL, due to less harm being caused and fewer unplanned admissions. There was also up to 15 minutes consultant administrative time saved per patient per triage, which can be used for clinical duties; as well as a 27% reduction in 52-week waiters during the first six weeks of deployment.
Nationally, there are 396,123 patients waiting to start treatment in the NHS for cardiology, with 31,689 waiting to start treatment over 41 weeks, 3,302 of these patients are waiting over 52 weeks. If the same 27% reduction seen in Cheshire and Merseyside was applied nationally, it could potentially reduce the national waiting list for patients waiting over 52 weeks by 891 patients within the first six weeks of deployment.
PRO-MAPP – Digital support tool for transforming preoperative assessment
PRO-MAPP is an intelligent decision support tool that has transformed the preoperative assessment (POA) process in the pre-assessment clinical triage pathway for high volume, low complexity (HVLC) orthopaedic cases.
The tool enables efficient triage by determining whether a face-to-face or telephone assessment is necessary, optimising the allocation of resources.
Implementing PRO-MAPP at the Nuffield Orthopaedic Hospital resulted in a 70% reduction in face-to-face pre-surgery appointments. Without surgical complexity, these patients feed directly into designated HVLC operating lists.
In December 2023, 120,277 patients started admitted treatment for surgical services in England. If PRO-MAPP had delivered the same results on a national scale, 92,000 of these patients could have been effectively assessed over the phone and unnecessary face-to-face appointments avoided during the demanding winter period.
If the same 70% reduction in face-to-face appointments could be achieved nationally, for trauma and orthopaedic services alone this could mean 27,298 fewer face-to-face appointments per month, with a potential cost saving of between £4.1M and £20.9M using PRO-MAPP, per month.
Lenus Health – Predictive AI for Chronic Conditions OPERA Study
Lenus Health provides AI and digital tools to existing care pathways to improve healthcare delivery, reduce admissions and improve outcomes. The Lenus platform focuses on transforming diagnosis pathways, which supports both Urgent and Emergency Care (UEC) recovery by avoiding admissions of undiagnosed patients, and elective care recovery by reducing waiting lists and improving patient experience.
This service began in cardiology where it evidenced a 78% reduction in time to diagnosis for heart failure patients using its digital pathway product.
To date, Lenus has supported more than 17,500 people in the UK and launched the world’s first predictive AI in the direct care of patients with chronic conditions.
Get in touch with your local health innovation network to find out more about what innovations are available to you to help you with your productivity challenges.

Join us on 11 and 12 June in Manchester to find out how the Health Innovation Network is improving health and driving wealth through health innovation. This year we’ll be joined on our stand by 18 Network-supported innovators, showcasing innovations which are helping to deliver the Government’s three shifts for the NHS and solve some [...]

The Health Innovation Network is delighted to announce the launch of Innovation Insights, a brand-new webinar series designed to highlight the latest in health innovation, offering attendees valuable insights into the adoption and spread of innovation within the health and care landscape. Each interactive webinar will feature: Expert presentations: Delivered by thought leaders across [...]

The Health Innovation Network, at an event sponsored by Sarah Coombes MP, brought together parliamentarians including Health Minister Karin Smyth MP and Chair of the Science, Innovation and Technology Committee, Chi Onwurah MP to meet with six innovators supported by health innovation networks across the country and their NHS partners. At the Meet the Innovators: [...]