How the Health Innovation Network is improving outcomes for premature babies
Nearly 58,000 babies are born prematurely in the UK every year, according to estimates by charity Bliss. This means that 1 in every 13 babies in the UK are born before 37 weeks of pregnancy. Not all premature babies need specialist neonatal care, but prematurity is associated with behavioural difficulties, long-term health problems and cerebral palsy.
The Health Innovation Network supports the delivery of the Maternity and Neonatal Safety Improvement Programme (MatNeoSIP), as part of the National Patient Safety Improvement Programme, through its 15 regional Patient Safety Collaboratives (PSCs).
To mark World Prematurity Day we are highlighting projects from across the Network that are improving outcomes for babies born prematurely.
Health Innovation Manchester: Supporting local maternity and neonatal teams in increasing the number of premature babies with an ideal body temperature on admission to neonatal care
Babies born at under 34 weeks gestation are at increased risk of hypo (low) and hyper (higher) thermia (temperature) due to their:
- Large surface area to body mass ratio
- Reduced skin thickness
- Poorly developed metabolic mechanisms.
It is crucial that these babies have a normal temperature range (36.5 – 37.5°c) on admission to the neonatal unit, that has been measured within one hour of birth. Research has shown that ensuring babies have a normal temperature will reduce the incidence of neonatal mortality, brain haemorrhage, necrotising enterocolitis, and sepsis. Additionally, there is emerging evidence that links early hyperthermia (above 38°c) with adverse outcomes too.
Within maternity and neonatal care there are many initiatives being used to maintain or increase a baby’s temperature to its ideal level, from maternal skin-to-skin contact for late preterm babies to Neohelp heat regulation suits, and transwarmers for our extreme preterm babies.
One initiative that has seen a big impact for Greater Manchester preterm babies and has been developed by Wythenshawe Hospital is called TOAST (Temperature On Arrival, Stay Thermoneutral). The TOAST care bundle is designed to improve thermal care of very preterm babies (under 32 weeks). This is achieved by the allocation of a dedicated ‘thermal care nurse’, a thermal care checklist to aid a standardised approach, and a rolling education programme for doctors and nurses to make them aware of the need to ensure an ideal temperature for all pre-term babies.
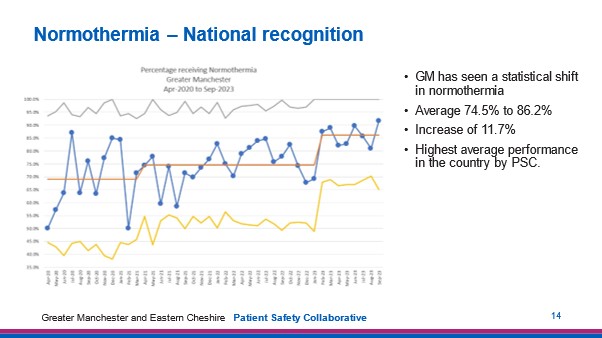
Greater Manchester maternity and neonatal teams have received national recognition for the normothermia (ideal temperature) measure. Figures show the highest national average increase (11.7%) of babies with a normal temperature. This means that now 86.2% of all Greater Manchester preterm babies born have the normal temperature range – giving them a better start to their early lives.
Find out more about how the Health Innovation Manchester PSC is supporting the national Maternity and Neonatal Safety Improvement Programme: Health Innovation Manchester MatNeoSIP.
Health Innovation Wessex: Supporting collaboration with parents and staff to increase the availability of breastmilk for preterm babies within 24 hours of birth
Babies admitted to neonatal intensive care are often born prematurely and may be unable to breastfeed straight away. Receiving colostrum (first milk) ensures that babies receive antibodies, protects their immature digestive system, and improves long term outcomes. Supporting parents during the first few days after a baby is born improves outcomes too.
With this in mind, Portsmouth Hospitals University asked parents and staff what support they felt they needed for milk production, their mental wellbeing, and to improve their overall experience. Staff were also asked to identify any barriers to support. This is part of a wider ‘Pathway to Excellence Preterm Birth Optimisation’ initiative.
Collaborating with parents and staff has resulted in the hospital establishing:
- A neonatal feeding team
- 7-day a week support with link nurses lead by International Board-Certified Lactation Consultants
- Tailored action plans
- Improved communication between maternity and neonatal intensive care unit (NICU) teams
- A commitment to the UNICEF Baby Friendly initiative
- An ‘all through’ journey, improving communication pathways between services
- Readily available equipment and resources.
It is well documented that 70% of the variance between the lowest and highest performing teams correlates to the quality of relationships between every team member. To deliver the quality improvements to the best of the unit’s ability, the team underwent a coaching programme with support from the Health Innovation Wessex PSC. The coaching supported the team on their journey of implementing early breastmilk and in-labour antibiotics for preterm babies as local priorities within the MatNeoSIP preterm optimisation pathway.
Looking ahead, Portsmouth Hospitals University is planning activities and events to build on its joint compassionate and supportive culture across maternity and NICU teams.

Portsmouth Hospitals University NHS Trust NICU and Maternity team members.
Midwife Nicola Keefe commented:
“Neonatal and maternity have come together as a team to improve preterm outcomes. The collaboration ‘Pathway to Excellence Preterm Birth Optimisation’ was introduced earlier this year. The aim of this pathway is to increase positive outcomes by identifying pregnancies at risk of preterm birth with an aim to preventing them and optimising the wellbeing of the baby and family when preterm birth is unavoidable… This collaboration has not only brought us together and improved preterm services, but the relationships between staff across NICU and Maternity.”
Find out more about how the Health Innovation Wessex PSC is supporting the national Maternity and Neonatal Safety Improvement programme: Health Innovation Wessex MatNeoSIP.
Health Innovation South West and Health Innovation West of England: A bundle of care to improve outcomes for premature babies
Preterm birth is the main cause of neonatal deaths and morbidity in the UK. While survival rates are improving, there is a growing population of children with neuro-disabilities due to premature birth.
PERIPrem is a unique care bundle of 11 interventions proven to have an impact on brain injury and mortality rates amongst babies born before 34 weeks.
The bundle was developed collaboratively by Health Innovation West of England, Health Innovation South West, and the South West Neonatal Network. Since April 2020, they have been supporting all 12 hospital trusts across the South West region to use the care bundle.
Quality improvement (QI) methodology has been central to implementation, alongside coaching and forging new ways of working, enabling obstetrics, midwifery and neonatal clinicians to join forces to transform care.
By August 2023, over 2,299 premature babies have been cared for using the PERIPrem bundle.
The National Neonatal Audit Programme’s (NNAP) 2022 report (published in November 2023) shows:
- The South West Neonatal Operational Delivery Network (ODN) has the lowest rates of severe preterm white matter brain injury or death
- The South West is the top ODN for early breastmilk feeding and delayed cord clamping
- Optimal place of birth is above average across the South West (80.4%) and is the only ODN in England demonstrating consistent improvement in this area during 2020-2022.
Perinatal team culture has also improved, with an enhanced common language and situational monitoring, according to an independent evaluation of PERIPrem conducted by Health Innovation South West in 2022. Staff are empowered to increase their knowledge, skills and confidence in preterm birth and infant care, benefitting from strategic cues, protected time, and access to tailored resources and QI support.
The third update to the Saving Babies’ Lives Bundle, published in June 2023, encourages providers of maternity and neonatal care to draw upon the learning of PERIPrem to aid the optimisation of perinatal care, while our PERIPrem resources have also received Neonatal Nurses Association (NNA) endorsement.
Dr Karen Luyt is Professor of Neonatal Medicine at the University of Bristol and is PERIPrem’s Clinical Strategic Lead. She said:
“The South West units have led the way in many of the NNAP quality metrics in 2022. We have for the last three years improved continuously with optimal place of birth for extremely preterm infants and if we can continue on this trajectory, we can enable still more babies to survive free from brain injury.
“The NCMD data return for 2021/2022 ranks the South West as the English region with the lowest neonatal mortality rate, which reflects the impact of our PERIPrem QI collaborative and the stellar efforts of every one of our 12 perinatal teams.”
There has been great interest in PERIPrem following its success in the South West. PERIPrem Cymru launched in Wales in 2023, supported by Health Innovation West of England through the sharing and adapting of resources developed during the initial project.
Find out more about PERIPrem and download useful resources.
Find your local Health Innovation Network to discuss support for maternity and neonatal safety in your area.
See the latest update of the Health Innovation Network patient safety plan showing the impact made across priority areas.

Jo Barosa is Account Director at Qbtech UK. Qbtech is a market leading provider of innovative objective tests for assessing and treating ADHD, changing the landscape of ADHD care. Driven by its mission to improve the lives of people with ADHD, Qbtech supports by providing digital and clinical solutions to improve clinical decision making, service [...]

Dr Cheryl Crocker, interim Chief Operating Officer at the Health Innovation Network, explains the vital role innovation plays to not only reduce waiting lists and improve access to care, but to decrease system pressure by improving people’s health and keeping them well for longer. The new Government has rightly declared its focus on moving the [...]

Launched in 2014, SiSU Health is scaling early warning, self-service health kiosks, digital platforms and pathways into pre-existing healthcare services. The British Heart Foundation estimates the annual cardiovascular disease (CVD) related costs to the UK healthcare system are around £10 billion, with annual costs to the UK economy of an estimated £25 billion. Making the [...]